Discover a comprehensive treatment guide for Post-Infectious IBS, including dietary changes, medications, and lifestyle modifications to alleviate symptoms effectively in 2025.
Introduction
Post-Infectious Irritable Bowel Syndrome (PI-IBS) affects many individuals following a bout of gastroenteritis, leaving them with lingering gastrointestinal symptoms. Did you know that approximately 10% of people develop PI-IBS after an episode of intestinal infection? This condition can lead to chronic discomfort, including diarrhea, bloating, and abdominal pain. Luckily, effective treatment strategies are available! In this guide, we’ll explore various approaches to managing PI-IBS, focusing on dietary changes, medications, and lifestyle adjustments that can help restore your gut health and improve your quality of life.
Understanding Post-Infectious IBS
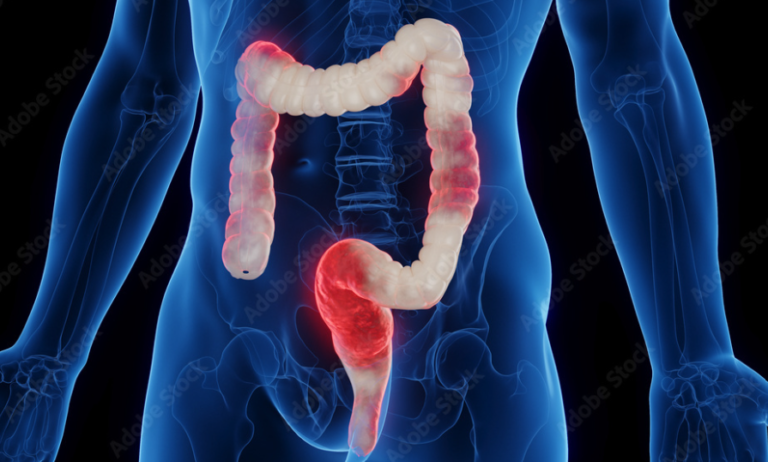
Definition: Post-Infectious IBS is characterized by persistent gastrointestinal symptoms following an acute infectious gastroenteritis episode. Symptoms may include abdominal pain, diarrhea, and bloating that continue long after the initial infection has resolved.
Causes: The condition often arises after infections caused by pathogens like Campylobacter, Salmonella, or Norovirus. These infections can lead to inflammation and changes in gut motility that trigger IBS symptoms.
Symptoms: Common symptoms of PI-IBS include cramping abdominal pain, frequent diarrhea (often urgent), bloating, and altered bowel habits. These symptoms may mimic those of typical IBS but often have a distinct onset related to prior infections.
Risk Factors for Developing PI-IBS
Infection Severity: The severity of the initial gastrointestinal infection plays a significant role in the likelihood of developing PI-IBS. More severe infections with extensive tissue damage are associated with a higher risk.
Demographic Factors: Studies indicate that women are more likely than men to develop PI-IBS. Age and psychological factors such as stress or anxiety during the infection can also influence outcomes.
Pre-existing Conditions: Individuals with a history of gastrointestinal disorders or those who have experienced multiple infections may be at greater risk for developing PI-IBS.
Dietary Approaches for Managing Symptoms
Low FODMAP Diet: Following a low FODMAP diet can significantly reduce symptoms for many individuals with PI-IBS. This diet restricts fermentable carbohydrates that can exacerbate bloating and gas.
Elimination Diets: Identifying and eliminating specific food intolerances or sensitivities can help manage inflammation in the gut. Foods commonly eliminated include gluten, dairy, and certain high-sugar items.
Increased Fiber Intake: Incorporating soluble fiber into the diet can help regulate bowel movements and improve overall gut health. Sources include oats, psyllium husk, and fruits like bananas and apples.
Medications for Symptom Relief
Antidiarrheal Agents: Medications like loperamide can provide quick relief from diarrhea by slowing down gut motility. These are often recommended for individuals experiencing frequent loose stools.
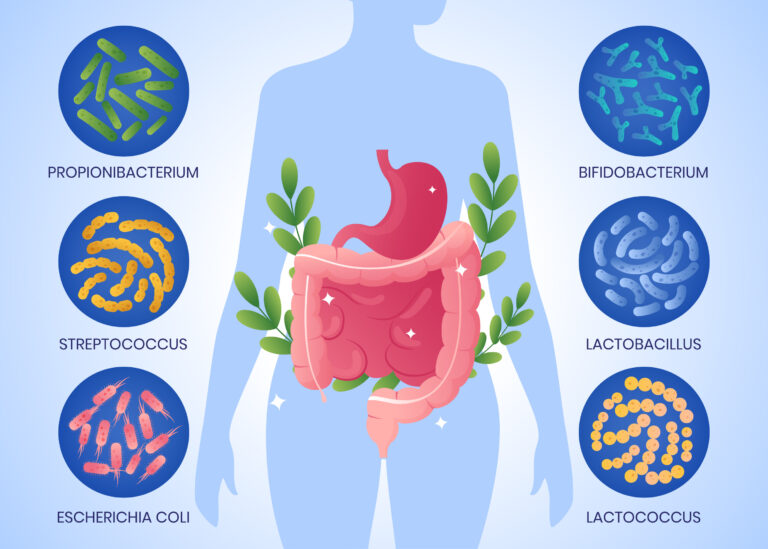
Probiotics: Research suggests that probiotics can help restore gut flora balance disrupted by infections. Specific strains may be beneficial in reducing IBS symptoms.
Antidepressants: Low-dose tricyclic antidepressants like amitriptyline may help alleviate pain and improve bowel function by modulating gut sensitivity and motility.
Lifestyle Modifications for Better Management
Stress Management Techniques: Stress has been shown to exacerbate IBS symptoms. Techniques such as mindfulness meditation, yoga, or cognitive behavioral therapy can be effective in managing stress levels.
Regular Exercise: Engaging in regular physical activity can promote healthy digestion and reduce stress. Activities like walking, swimming, or cycling are excellent choices.
Adequate Hydration: Staying hydrated is crucial for digestive health. Drinking plenty of water helps maintain bowel regularity and supports overall well-being.
Monitoring Symptoms and Progress
Keeping a Symptom Diary: Documenting food intake alongside symptom occurrences can help identify triggers and patterns in your condition. This information is invaluable when discussing treatment options with healthcare providers.
Regular Follow-ups with Healthcare Providers: Ongoing communication with your doctor or gastroenterologist is essential for managing PI-IBS effectively. Regular check-ups allow for adjustments in treatment plans based on symptom progression.
Conclusion:
Post-Infectious IBS can be a challenging condition to manage after an acute gastrointestinal infection. However, with the right combination of dietary adjustments, medications, and lifestyle changes, many individuals find significant relief from their symptoms. Remember to consult healthcare professionals for personalized advice tailored to your situation. Start implementing these strategies today to reclaim your digestive health!