Discover the symptoms, diagnosis, and management strategies for sucrose intolerance in adults. Learn how to identify and effectively navigate this complex digestive disorder.
Introduction:
Adult sucrose malabsorption is a real challenge for many adults! Did you know that approximately 1 in 5,000 people struggle with this often misunderstood digestive disorder? When your body can’t properly break down sugar, every meal becomes a potential minefield of uncomfortable symptoms. In this comprehensive guide, we’ll dive deep into the world of adult sucrose malabsorption, helping you understand what’s really going on in your digestive system.
What is adult sucrose malabsorption?
Definition of adult Sucrose Malabsorption
Adult sucrose malabsorption is a digestive disorder characterized by the body’s inability to effectively break down and absorb sucrose (table sugar). This occurs due to a deficiency or complete absence of the sucrase enzyme, which is responsible for splitting sucrose into its component simple sugars: glucose and fructose.
Difference Between Sucrose Intolerance and Other Sugar-Related Digestive Issues
Sucrose intolerance stands apart from other sugar-related digestive disorders in several key ways. While lactose intolerance involves the inability to break down milk sugar (lactose) due to a lactase enzyme deficiency, sucrose intolerance specifically targets table sugar through a lack of the sucrase enzyme.
Unlike fructose malabsorption, which affects the body’s ability to process fruit sugar and involves issues with GLUT5 transporters, sucrose intolerance stems from the inability to break down the chemical bond between glucose and fructose molecules in sucrose.
This condition isn’t a general sensitivity to all sugars, but rather a precise enzymatic deficiency that can be either inherited through genetic mutations or acquired through intestinal damage or disease. The specificity of this enzyme deficiency makes it a distinct metabolic condition that requires targeted treatment approaches, setting it apart from broader sugar sensitivities or general digestive issues. Understanding these differences is crucial for proper diagnosis and management, as treatment strategies vary significantly between different types of sugar intolerances.
Genetic and Acquired Causes
Genetic Causes:
– Congenital sucrase-isomaltase deficiency (CSID)
– Inherited as an autosomal recessive trait
– Present from birth
– Caused by mutations in the SI gene
Acquired Causes:
Chronic intestinal diseases
Surgical interventions
Severe gastrointestinal infections
Inflammatory bowel conditions
Age-related enzyme production decline
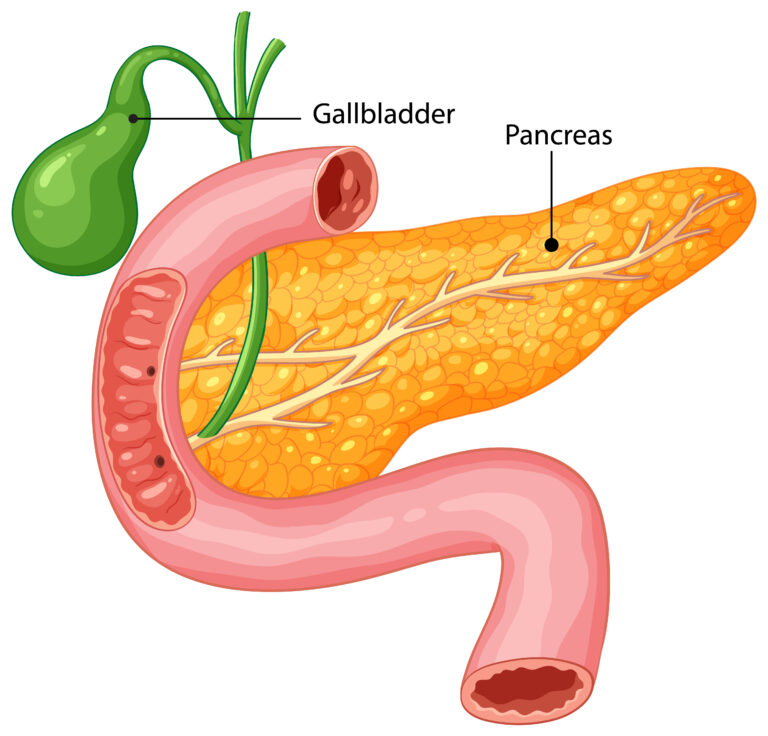
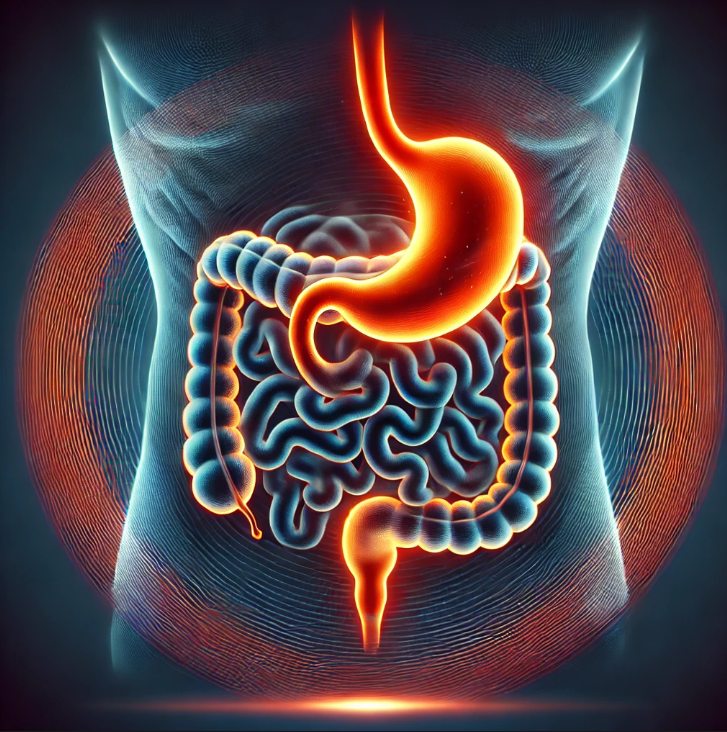
How the Digestive System Processes Sucrose Normally
1- Sucrose enters the small intestine during digestion
2- Sucrase enzyme located in intestinal brush border
3- Enzyme splits sucrose into glucose and fructose
4- Simple sugars absorbed through intestinal wall
5- Transported to liver via bloodstream
6- Metabolized for energy or stored
Key Physiological Steps:
– Enzymatic breakdown
– Absorption through intestinal epithelium
– Metabolic processing
– Energy conversion
Symptoms of adult sucrose malabsorption
Digestive Warning Signs
– Explosive, watery diarrhea
– Severe abdominal cramping
– Excessive gas and bloating
– Rumbling/gurgling sounds in abdomen
– Nausea after sugar consumption
read more about IBS, SIBO management strategies.
Gastrointestinal Distress Indicators
– Chronic loose stools
– Sharp, intermittent stomach pain
– Rapid transit time of food
– Urgent bowel movements
– Rectal urgency
– Potential weight loss
Long-Term Health Implications
– Potential nutrient malabsorption
– Electrolyte imbalances
– Chronic malnutrition risks
– Compromised gut microbiome
– Increased intestinal permeability
– Potential development of secondary conditions
Variations in Symptom Severity
Mild: Occasional digestive discomfort
Moderate: Predictable symptoms after sugar intake
Severe: Debilitating gastrointestinal responses
Episodic vs. consistent symptoms
Individual metabolic variations
Distinguishing from Other Digestive Disorders
Differential Diagnosis Indicators:
Timing of symptoms post-sugar consumption
Specific sugar triggers
Absence of inflammatory markers
Genetic testing confirmation
Response to enzyme supplementation
Distinct from IBS, lactose intolerance, celiac disease
Diagnosis and Medical Testing
Diagnostic Criteria
– Persistent digestive symptoms after sugar intake
– Confirmation through specialized testing
– Ruling out alternative digestive disorders
– Age and symptom onset documentation
Hydrogen Breath Test Procedures
Patient consumes sucrose solution
Breath samples collected at intervals
Measures hydrogen production
Indicates malabsorption levels
Non-invasive diagnostic method
Blood and Genetic Testing Methods
Genetic sequencing for SI gene mutations
Enzyme activity blood panels
Genetic inheritance pattern analysis
Congenital Sucrase-Isomaltase Deficiency (CSID) screening
DNA testing for specific genetic markers
Role of Medical History in Diagnosis
Family digestive disorder history
Detailed symptom tracking
Dietary intake documentation
Previous gastrointestinal conditions
Ethnicity-related genetic predispositions
Challenges in Accurate Diagnosis
Symptom overlap with other disorders
Limited clinical awareness
Complex genetic testing requirements
Variability in symptom presentation
Potential misdiagnosis risks
Need for comprehensive multi-stage evaluation
Dietary Management Strategies
Complete and Partial Sucrose Elimination Diets
Total sugar elimination approach
Gradual reduction strategies
Reading food labels carefully
Identifying hidden sugar sources
Developing personalized dietary plan
Alternative Sugar Sources
Stevia
Monk fruit sweeteners
Sugar alcohols (xylitol, erythritol)
Natural low-sucrose sweeteners
Glucose-based alternatives
Nutritional Considerations
Balanced macronutrient intake
Micronutrient supplementation
Protein and fat emphasis
Complex carbohydrate selection
Maintaining caloric requirements
Enzyme Replacement Options
Sucrase enzyme supplements
Prescription enzyme medications
Over-the-counter digestive aids
Timing of enzyme intake
Dosage management strategies
Working with a Registered Dietitian
Personalized nutrition planning
Symptom tracking
Meal preparation guidance
Nutritional gap identification
Long-term dietary management
Living with Sucrose Malabsorption
Lifestyle Adaptations
Strict dietary monitoring
Meal planning and preparation
Carrying emergency enzyme supplements
Learning food ingredient translations
Developing cooking skills for alternative recipes
Mental Health Considerations
Addressing potential dietary frustration
Developing coping mechanisms
Managing stress related to dietary restrictions
Psychological impact of chronic condition
Building resilience and positive mindset
Long-Term Health Management
Regular medical follow-ups
Continuous nutritional monitoring
Genetic counseling
Emerging treatment research tracking
Holistic health approach integration
Conclusion
Living with sucrose intolerance isn’t a limitation – it’s an opportunity to understand your body better! By implementing strategic dietary choices, working closely with healthcare professionals, and staying informed, you can effectively manage this condition and maintain excellent quality of life.