Explore the key differences between GERD and acid reflux, including symptoms, causes, and treatments. Learn how to manage each condition effectively with diet and lifestyle tips to reduce discomfort and improve quality of life.

Introduction:
Understanding whether you’re dealing with GERD or simple acid reflux can be challenging, yet it’s crucial for effective management. While both conditions share similarities, they require different treatment approaches. Did you know that nearly 20% of adults in the U.S. experience GERD symptoms weekly? By distinguishing between GERD and acid reflux, you’ll be better equipped to manage symptoms, avoid triggers, and improve your health. Let’s dive into what makes these conditions unique and how you can confidently tackle each one!
What Is Acid Reflux?
It is a condition where stomach acid flows back into the esophagus, causing that uncomfortable burning sensation we call heartburn. It’s like your stomach is throwing a little party, and your esophagus wasn’t invited! But don’t worry, we’ll chat about how to calm things down.
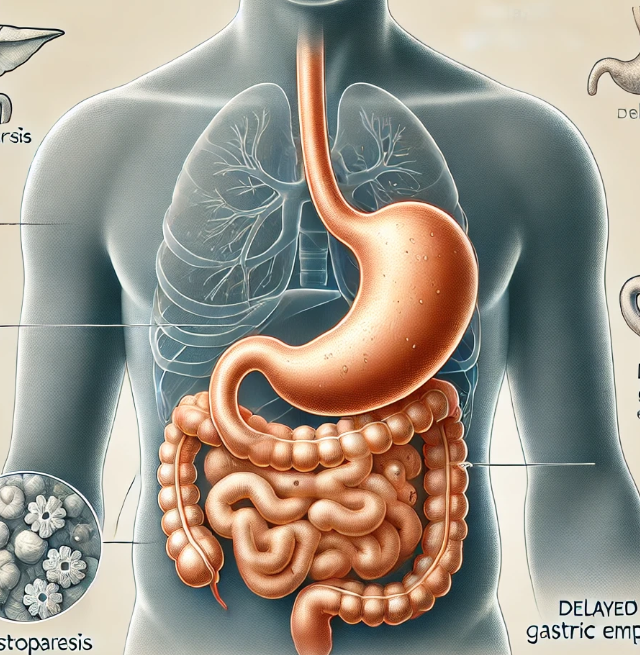
Scientifically talking, Acid reflux happens when the sphincter muscle at the lower end of the esophagus relaxes at the wrong time, allowing stomach acid to back up into the esophagus.
Typical symptoms of acid reflux can vary from Regurgitation and heartburn to chest discomfort.
– Duration of Symptoms: Symptoms can be short-lived, often lasting from a few minutes to a few hours. Dietary choices (such as fatty or acidic foods), large meals, or lying down soon after eating can trigger these episodes.
-Lifestyle Factors Contributing to Acid Reflux:
Dietary Choices: Fatty or Fried Foods: These can slow gastric emptying and relax the LES, promoting acid reflux.
Citrus Fruits and Tomatoes: High in acid, these foods can irritate the esophagus and increase reflux.
Chocolate and Mint: Both can relax the LES, making it easier for acid to escape from the stomach.
Spicy Foods: Often trigger heartburn and reflux symptoms, especially in sensitive individuals.
Caffeinated and Carbonated Beverages: Coffee, tea, soda, and other caffeinated drinks can relax the LES and increase acid production.
Alcohol: Relaxes the LES and may increase stomach acid production, leading to reflux.
Meal Timing and Size: Large Meals: Eating a lot at once puts pressure on the LES and increases the chance of reflux.
Eating Late at Night: Lying down soon after a meal can encourage acid to move up the esophagus, especially if the LES is relaxed.
Body Position and Posture: Lying Down After Eating: Horizontal positioning makes it easier for acid to escape into the esophagus, so it’s best to wait at least 2-3 hours after a meal.
Bending Over: This can increase abdominal pressure, pushing acid up.
Weight and Obesity: Excess weight, especially around the abdomen, increases pressure on the stomach and LES, making reflux more likely.
Smoking: Nicotine weakens the LES and also stimulates acid production. Chronic smoking can also lead to other structural changes that increase acid reflux.
Medications: Certain medications can increase acid reflux risk. These include NSAIDs (like ibuprofen and aspirin), certain blood pressure medications (such as calcium channel blockers), and some muscle relaxants. Always check with a healthcare provider if symptoms worsen after starting a new medication.
What Is GERD (Gastroesophageal Reflux Disease)?
GERD, which stands for Gastroesophageal Reflux Disease, is a long-lasting digestive problem. It happens when the food and acid from your stomach often come back up into your food pipe (esophagus). This occurs because a muscle at the bottom of your food pipe, called the lower esophageal sphincter (LES), isn’t working properly. Normally, this muscle acts like a door, keeping stomach contents from flowing back up.
-Symptoms:
GERD presents a range of symptoms that extend beyond typical acid reflux. Primary symptoms include heartburn, regurgitation, difficulty swallowing, and the sensation of food stuck in the throat. Additionally, GERD can manifest extra-esophageal symptoms such as chronic cough, hoarseness, and dental erosion. Risk factors for GERD are multifaceted, encompassing lifestyle choices like obesity and smoking, medical conditions including pregnancy and hiatal hernia, and other factors such as age and family history. Understanding these symptoms and risk factors is crucial for effective management and treatment of GERD.
Key Differences Between Acid Reflux and GERD
While many people experience occasional acid reflux:
Occasional reflux: Happens sporadically, often after large meals or trigger foods
GERD: Occurs at least twice per week for several weeks
GERD symptoms are more severe and can significantly impact quality of life
GERD can cause tissue damage in the esophagus over time
Duration and Frequency Acid Reflux:
-Occurs occasionally, often triggered by specific foods or activities
-May happen a few times per month
-Generally resolves on its own or with over-the-counter remedies
-Often predictable based on eating patterns or activities
GERD:
-Occurs regularly (at least twice weekly)
-Persists for extended periods (3+ months)
-Requires ongoing management
-May occur regardless of dietary choices or lifestyle modifications
Symptom Severity and Impact Acid Reflux:
Mild to moderate discomfort
Minimal interference with daily activities
Usually manageable with lifestyle changes
Rarely disrupts sleep patterns
GERD:
More intense symptoms
Significant impact on quality of life
Can interfere with work and social activities
Often disrupts sleep
May require dietary restrictions
Can affect emotional well-being
Long-term Health Risks of Untreated GERD
Esophageal complications: Barrett’s esophagus (precancerous changes), esophageal strictures (narrowing), Esophagitis (inflammation), Potential for esophageal cancer
Respiratory complications: Chronic cough, Asthma exacerbation, Recurrent pneumonia, Voice changes
Dental complications: Tooth enamel erosion, Increased cavity risk, Gum disease
Diagnostic criteria:
Frequency of symptoms
Presence of complications
Impact on quality of life
Response to treatment
Causes of Acid Reflux and GERD: What’s the Same, What’s Different?
Acid reflux and GERD share several common causes, often rooted in dietary, lifestyle, and physical factors. Dietary triggers include consuming large portion sizes, high-fat, spicy, or acidic foods, and specific irritants like chocolate, citrus fruits, tomato-based products, mint, coffee, and carbonated drinks.
Lifestyle habits also play a role, such as eating close to bedtime, lying down soon after meals, wearing tight-fitting clothing, smoking, alcohol consumption, and experiencing high stress levels. Physical conditions like obesity, pregnancy, and poor posture during meals can further exacerbate symptoms by increasing pressure on the stomach, contributing to the backward flow of stomach acid into the esophagus.
How Are Acid Reflux and GERD Treated?
Treating acid reflux and GERD often involves a range of options, tailored to the severity and frequency of symptoms. For occasional acid reflux, over-the-counter antacids and H2 blockers (such as ranitidine or famotidine) are commonly used to neutralize stomach acid or reduce its production. However, for chronic cases of GERD, treatment typically includes proton pump inhibitors (PPIs) like omeprazole or esomeprazole, which offer longer-lasting acid suppression. In severe or refractory cases, surgical interventions such as fundoplication may be recommended to strengthen the lower esophageal sphincter and prevent acid from refluxing.
Given the chronic and progressive nature of GERD, the treatment approach differs in its focus on longer-term management to prevent complications like esophagitis or Barrett’s esophagus. In contrast, acid reflux treatments often aim for quick, short-term relief.
Regardless of diagnosis, lifestyle and dietary modifications are essential for both conditions. Patients are advised to avoid dietary triggers, eat smaller meals, manage weight, and refrain from lying down after eating. Such adjustments are foundational, as they can significantly reduce the frequency and intensity of reflux episodes.
Diet and Lifestyle Changes for Managing GERD and Acid Reflux
Managing GERD and acid reflux effectively often begins with diet and lifestyle modifications. Certain foods are known to trigger reflux and should be minimized or avoided, including caffeine, spicy foods, fatty meals, chocolate, alcohol, and acidic foods like citrus fruits and tomatoes.
Adjusting meal portions and timing also helps, as eating smaller, more frequent meals and avoiding food intake at least two to three hours before lying down can reduce symptoms significantly. Maintaining a healthy weight is essential, as excess weight places additional pressure on the stomach, promoting acid reflux.
Additionally, wearing loose-fitting clothing, especially around the abdomen, can help alleviate discomfort. GERD-specific recommendations may also include elevating the head of the bed or using a wedge pillow to prevent nighttime reflux by keeping acid below the esophagus. Together, these modifications can be powerful strategies for reducing the frequency and intensity of acid reflux and GERD symptoms.
Long-term Management: Preventing Complications of GERD
Effective, long-term management of GERD is essential to prevent serious complications that may arise if the condition remains untreated. Chronic acid exposure can lead to inflammation of the esophagus, increasing the risk of conditions such as Barrett’s esophagus—a precancerous change in the esophageal lining—and even esophageal cancer in severe cases. Regular medical evaluations, including endoscopies for high-risk individuals, are crucial for early detection of these complications.
Long-term management of GERD emphasizes consistent lifestyle adjustments, such as adhering to dietary guidelines, maintaining a healthy weight, and avoiding factors that exacerbate reflux symptoms. Ongoing treatment with medications like PPIs may be recommended to keep acid levels under control and protect the esophageal lining. By following these strategies and scheduling periodic check-ups, patients with GERD can manage symptoms effectively, maintain a high quality of life, and reduce the risk of serious complications.
Conclusion:
Understanding the differences between GERD and acid reflux can empower you to make informed decisions about managing symptoms and improving your health. Whether you experience occasional acid reflux or struggle with chronic GERD, adopting effective treatments and lifestyle changes is key to reducing discomfort and preventing complications. Remember, if symptoms persist, consult a healthcare provider to explore the best treatment options for you. Ready to take control of your digestive health? Start implementing these strategies today!