Discover the crucial gut health perimenopause warning signs women should be aware of in 2024. Learn how hormonal changes affect digestion and what steps to take for better gut health.

Introduction
Perimenopause is a time of significant hormonal shifts, and many women may not realize just how much these changes impact gut health! Did you know that fluctuating estrogen levels can trigger digestive issues like bloating and constipation? As you navigate perimenopause, being aware of gut health warning signs is key to maintaining your overall well-being. In this guide, we’ll break down the most common digestive symptoms you might experience and what they mean for your health. Let’s explore how to stay ahead of these issues in 2024.
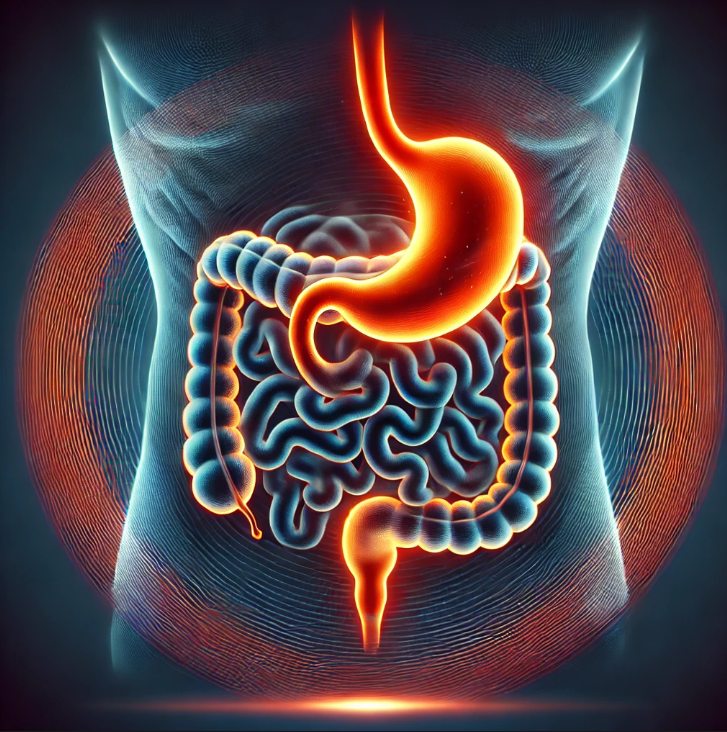
What Is Perimenopause and How Does It Affect Your Gut?
Perimenopause is the transitional phase leading up to menopause, often beginning in a woman’s 40s and lasting for several years. During this period, the ovaries gradually produce less estrogen and progesterone, leading to various physical and emotional changes. One area that is particularly affected by these hormonal shifts is the digestive system.
Estrogen plays a key role in maintaining gut motility, which is the process of moving food through the digestive tract. When estrogen levels fluctuate, it can slow down or speed up digestion, causing symptoms like bloating, gas, and constipation. Progesterone, another hormone that declines during perimenopause, has a relaxing effect on smooth muscles, including those in the digestive tract. As progesterone levels drop, women may experience increased bloating and slower digestion.
Additionally, perimenopause can disrupt the gut-brain axis, the communication network between the gut and brain, which can lead to increased sensitivity to stress and anxiety—factors that further impact digestion.
The hormonal rollercoaster also affects the gut microbiome, the community of bacteria and other microorganisms living in the digestive system. Research has shown that hormonal changes can alter the balance of “good” and “bad” bacteria in the gut, contributing to symptoms like indigestion, nausea, and even diarrhea. This complex interplay of hormones and gut health highlights the importance of being mindful of digestive changes during perimenopause, as the gut can often be an early indicator of hormonal imbalance.
Key Gut Health Warning Signs to Watch For
During perimenopause, hormonal fluctuations can trigger several gut health issues. Common warning signs include bloating and gas, caused by slower digestion due to reduced estrogen. Constipation is another frequent symptom, as declining estrogen and progesterone slow gut motility. Conversely, some women may experience bouts of diarrhea when hormone changes speed up digestion. Indigestion and nausea are also common, often linked to increased gut sensitivity during this time. These signs of digestive imbalance are important to monitor, as they often reflect the broader hormonal shifts impacting overall health during perimenopause.
Perimenopause Gut Health Tracking template for different symptoms:
Symptom tracking is a powerful tool for identifying patterns, understanding the root causes of issues, and helping healthcare providers make informed decisions. Below are detailed symptom tracking templates that focus on menopause digestive problems. These templates can be used daily or weekly to capture symptoms, intensity, frequency, and potential triggers.

Why Gut Health Matters During Perimenopause
- Nutrient Absorption: As women age and experience hormonal shifts, the body’s ability to absorb key nutrients such as calcium, magnesium, and B vitamins may be compromised. A healthy gut is vital for effective nutrient absorption, helping to support bone health and overall vitality during this critical phase.
- Immune Function: Approximately 70% of the immune system resides in the gut. A healthy gut microbiome supports immune function, helping to protect against infections and inflammation. This is particularly important during perimenopause when hormonal changes can lead to increased susceptibility to illness.
- Metabolic Health: Weight Management: Hormonal changes during perimenopause can lead to weight gain and changes in body composition. A healthy gut microbiome can influence metabolism and appetite regulation, helping to mitigate weight gain during this transitional period. – Blood Sugar Control: Gut health plays a role in insulin sensitivity and blood sugar regulation. Maintaining a balanced gut can help manage energy levels and reduce the risk of developing insulin resistance, which is crucial during perimenopause.
- Chronic Disease Prevention: Gut health is linked to various chronic diseases, including heart disease and osteoporosis. By supporting gut health during perimenopause, women can potentially reduce their risk of these conditions later in life.
- Hormonal Regulation: Estrogen influences gut microbiota, the community of microorganisms in the digestive tract. During perimenopause, fluctuating estrogen levels can disrupt this balance, potentially leading to digestive issues like bloating and constipation. A healthy gut microbiome helps maintain hormonal balance, which is crucial during this transitional phase.
- Symptom Management: Digestive Symptoms: Women often experience gastrointestinal symptoms during perimenopause, including bloating, gas, and changes in bowel habits. Maintaining a healthy gut can alleviate these symptoms, improving quality of life. Mood Regulation: The gut-brain axis links gut health to mental well-being. A balanced gut microbiome can positively influence mood and anxiety levels, which may be heightened during perimenopause due to hormonal changes.
Natural Approaches to Support Gut Health
1- High-Fiber Diet:
Incorporate fruits, vegetables, whole grains, and legumes to promote healthy digestion and support beneficial gut bacteria.
2- Fermented Foods:
Include yogurt, kefir, sauerkraut, kimchi, and miso to enhance gut microbiota diversity and improve digestion.
3- Hydration:
Drink plenty of water to maintain gut motility and support overall digestive health.
4 Regular Physical Activity:
Engage in regular exercise to stimulate digestion, reduce stress, and enhance overall well-being.
5- Stress Management:
Practice mindfulness techniques such as yoga, meditation, or deep breathing exercises to reduce inflammation and support gut health.
6- Probiotics:
Consider taking probiotic supplements to promote a balanced gut microbiome, especially during hormonal changes.
7- Prebiotic Foods:
Include prebiotic-rich foods like garlic, onions, asparagus, and bananas to nourish beneficial gut bacteria.
8- Limit Processed Foods:
Reduce the intake of high-sugar and high-fat processed foods that can negatively impact gut health.
9- Avoid Overuse of Antibiotics:
Use antibiotics judiciously, as they can disrupt gut microbiota balance.
10- Mindful Eating:
Pay attention to hunger and fullness cues, and practice eating slowly to enhance digestion and nutrient absorption.
When to See a Doctor About Your Gut Health
It’s important to see a doctor about your gut health if you experience persistent or severe symptoms that could indicate an underlying issue.
Key signs include prolonged abdominal pain (more than 5 days), significant changes in bowel habits (such as chronic diarrhea or constipation), blood in your stool, unintentional weight loss, or persistent bloating that doesn’t improve with dietary changes.
Conclusion:
Gut health can easily get overlooked during perimenopause, but it plays a crucial role in your overall well-being. By recognizing the warning signs and taking proactive steps, you can manage digestive symptoms and ensure a smoother transition through perimenopause. Make 2024 the year you prioritize your gut health—starting today! Consult with your healthcare provider if any symptoms feel persistent or unusual. Your gut will thank you!