Explore the different types of colitis, their symptoms, causes, diagnosis, and treatment options. This comprehensive 2025 guide will help you understand how each type affects health and management strategies.
Introduction:
Did you know that colitis affects over 3 million Americans? (check out the whole statistics from here ) As someone who’s worked with gastroenterology patients for years, I’ve seen firsthand how overwhelming it can be to receive a colitis diagnosis. But here’s the good news – understanding your specific type of colitis is the first step toward effective management! In this comprehensive guide, we’ll explore the different forms of colitis, their unique characteristics, and the latest treatment approaches for 2025.
1. What is Colitis? Understanding the Basics
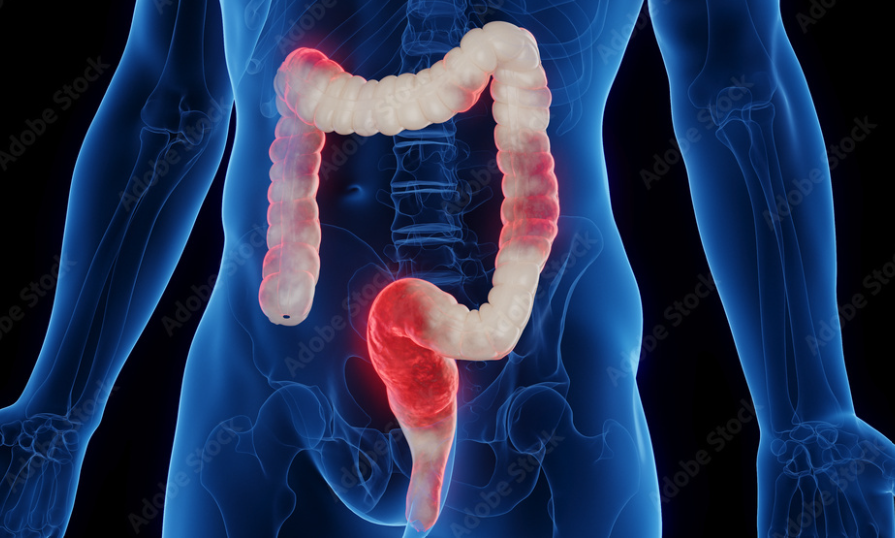
When your doctor mentions “colitis,” they’re referring to inflammation in your colon, also known as the large intestine. Picture your digestive system as a complex processing plant – your colon is the final quality control station, about 5 feet long, wrapping around your abdomen like a frame. While that might sound straightforward, understanding colitis is crucial because it affects nearly 3 million Americans each year!
The Digestive Detective: How Colitis Disrupts Your System
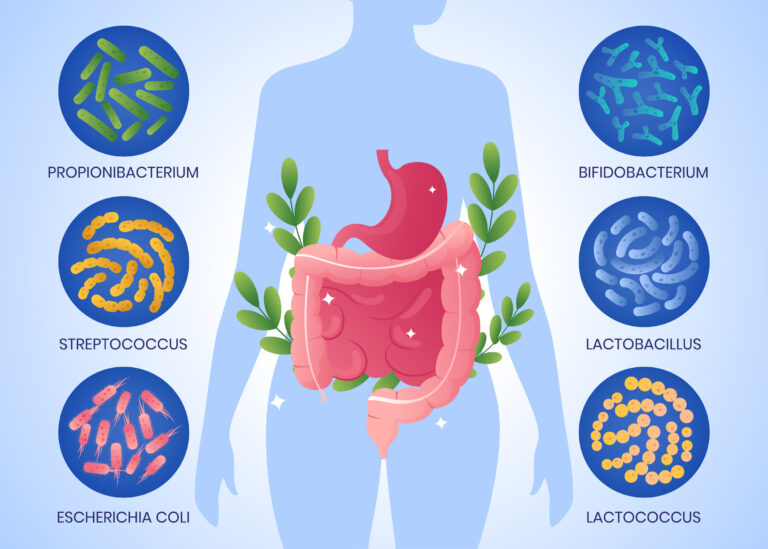
Your colon normally acts like a highly efficient recycling center. Its main job? Absorbing water from digested food, processing nutrients, and working with beneficial bacteria to maintain your gut health. But when colitis strikes, this well-oiled machine starts to malfunction. The inner lining of your colon becomes inflamed, much like a sunburn on the inside of your gut. This inflammation disrupts the delicate balance of your digestive system.
Think of your colon’s lining as a selective security barrier. When healthy, it knows exactly what to let through and what to keep out. But with colitis, this barrier becomes compromised. Water absorption goes haywire (hello, diarrhea!), nutrient processing becomes inefficient, and your gut bacteria – usually your faithful allies – might not function as they should.
Tale of Two Conditions: Acute vs. Chronic Colitis
Colitis isn’t a one-size-fits-all condition. Let’s break down the two main types you might encounter:
Acute colitis is like an unexpected house guest – it shows up suddenly and (thankfully) usually doesn’t stay long. Often triggered by infections, certain medications, or food poisoning, acute colitis typically resolves within a few days or weeks with proper treatment. It’s uncomfortable, yes, but usually temporary.
Chronic colitis, on the other hand, is more like that neighbor who moves in next door – it’s here to stay. This long-term condition often stems from autoimmune responses, where your immune system mistakenly attacks your own colon tissue. Chronic colitis typically follows a pattern of flare-ups (when symptoms are active) and remission periods (when symptoms calm down).
Risk Factors and Triggers: What Sets It Off?
Understanding what makes you more susceptible to colitis is like having a weather forecast for your gut. Several factors can increase your risk:
- Family history and genetics (thanks, Mom and Dad!)
- Age (it often debuts in your 20s and 30s)
- Geographic location (it’s more common in developed countries)
- Previous gastrointestinal infections
- Smoking (yet another reason to quit!)
As for triggers – those pesky factors that can set off symptoms – they’re like your colon’s personal nemeses:
- Certain foods (everyone’s triggers are different)
- Stress (your gut and brain are surprisingly chatty!)
- Some medications
- Poor sleep
- Hormonal changes
Quality of Life: The Real Impact
Living with colitis isn’t just about managing physical symptoms – it can feel like your entire life is getting a makeover you never asked for. The impact can ripple through various aspects of your daily routine:
- Physical activities might need modification
- Social plans might require careful planning (hello, bathroom mapping!)
- Work or school attendance might be affected
- Relationships might face new challenges
- Travel might need extra preparation
But here’s the empowering part: understanding these impacts is your first step toward managing them effectively. Many people with colitis lead full, active lives by learning their triggers, working closely with their healthcare team, and developing strong support systems.
Quick Fact Box:
Did you know? The gut has been called our “second brain” because it contains more nerve endings than the entire spinal cord! This explains why stress and emotions can significantly impact colitis symptoms.Warning Signs Box:
Seek immediate medical attention if you experience:
- Severe abdominal pain
- High fever
- Significant bleeding
- Severe dehydration
- Persistent vomiting
Remember, while colitis can be challenging, you’re not alone in this journey. Modern medicine continues to advance, offering better understanding and treatment options every year. The key is working with your healthcare provider to understand your specific type of colitis and develop a management plan that works for you.
2. Types of Inflammatory Bowel Disease (IBD) Related Colitis
When it comes to IBD-related colitis, we’re not just talking about one condition – we’re looking at several distinct types, each with its own characteristics and challenges. As a gastroenterology researcher recently noted, “Understanding the specific type of IBD-related colitis is crucial for proper treatment and management.” Let’s dive into each type to help you better understand these complex conditions.
Ulcerative Colitis: The Continuous Inflammation
Ulcerative colitis (UC) is like an unwanted artist, painting inflammation in one continuous stroke along your colon. Starting from the rectum, it can spread upward through the colon, creating a uniform pattern of inflammation. Here’s what makes UC unique:
– Pattern: The inflammation is continuous and uniform
– Location: Always affects the rectum and extends upward
– Depth: Only affects the innermost lining of the colon
– Pain: Often felt on the left side of the abdomen
– Bleeding: Common symptom due to surface ulcers
Key symptoms include:
– Bloody diarrhea (the hallmark sign)
– Urgent bowel movements
– Abdominal cramping
– Weight loss
– Fatigue
What causes UC? While the exact cause remains mysterious, it’s believed to be an autoimmune response gone wrong, with genetics and environment playing starring roles in this unwanted drama.
Crohn’s Colitis: The Skip Pattern Specialist
Unlike its cousin UC, Crohn’s colitis is more like a spots and patches kind of condition. It can affect any part of your digestive tract from mouth to bottom, but when it specifically affects the colon, we call it Crohn’s colitis. Here’s what makes it special:
– Pattern: “Skip lesions” – patches of healthy tissue between inflamed areas
– Depth: Can affect all layers of the intestinal wall
– Complications: May include fistulas and strictures
– Location: Can appear anywhere in the digestive tract
– Pain: Often felt on the right side or throughout the abdomen
Distinguishing features include:
– Patchy inflammation
– Deep ulcers
– Thickened intestinal wall
– Possible fistula formation
– Granulomas (visible under microscope)
Microscopic Colitis: The Hidden Challenger
Don’t let the name fool you – while microscopic colitis might be invisible to the naked eye, its impact is anything but tiny. This condition comes in two main flavors: lymphocytic and collagenous colitis. Think of it as the ninja of inflammatory bowel conditions – you can’t see it during a regular colonoscopy, but it’s definitely making its presence known!
Lymphocytic Colitis:
– Characterized by increased white blood cells in colon lining
– Typically affects middle-aged to older adults
– More common in women
– Main symptom: chronic watery diarrhea
– Normal-looking colon during colonoscopy
Collagenous Colitis:
– Features a thickened collagen band under the colon lining
– Similar age and gender preferences as lymphocytic
– Also causes chronic watery diarrhea
– Can be triggered by certain medications
– May come and go over time
Ischemic Colitis: The Senior Concern
Ischemic colitis is like a power outage in your colon – it occurs when blood flow to part of the colon is reduced, usually affecting older adults. This condition deserves special attention because it can be a medical emergency.
Key characteristics:
– Sudden onset of symptoms
– Usually affects people over 60
– Often related to blood vessel problems
– Can be triggered by low blood pressure
– May require immediate medical attention
Warning signs include:
– Sudden abdominal pain
– Urgent bowel movements
– Bloody diarrhea
– Tenderness in the abdomen
– Nausea and vomiting
IBD-Unclassified (IBDU): The Mystery Player
Sometimes, even with all our modern medical knowledge, colitis doesn’t fit neatly into any category – that’s where IBD-Unclassified comes in. It’s like having a puzzle piece that doesn’t quite match any specific spot but clearly belongs to the puzzle.
Characteristics of IBDU:
– Shows features of both UC and Crohn’s
– Diagnosis of exclusion
– May change over time
– Requires careful monitoring
– Treatment approach may be unique
Important Note
> Up to 15% of IBD cases are initially classified as IBDU. Some may later be diagnosed as either UC or Crohn’s as the disease pattern becomes clearer.
Treatment Approaches
While each type of IBD-related colitis requires its own specific treatment plan, some common approaches include:
– Anti-inflammatory medications
– Immune system suppressors
– Biologics
– Dietary modifications
– Lifestyle changes
– Surgery (when necessary)
Remember, proper diagnosis is crucial for effective treatment. What works for one type of colitis might not work for another, which is why working closely with a gastroenterologist is so important. They can help identify your specific type of colitis and create a treatment plan tailored to your needs.
Did You Know?
> Recent research shows that environmental factors, including diet, stress, and gut bacteria, play a significant role in all types of IBD-related colitis. Understanding these factors can help in managing your condition more effectively.
3. Non-IBD Forms of Colitis
While IBD-related colitis often takes the spotlight, there’s a whole other world of colitis types that aren’t related to inflammatory bowel disease. In fact, a recent medical survey showed that non-IBD colitis accounts for approximately 50% of all colitis cases! Let’s explore these different types and understand what makes each one unique.
Infectious Colitis: When Unwanted Guests Crash Your Gut Party
Infectious colitis is like having uninvited microscopic guests wreak havoc in your colon. It’s actually the most common form of colitis worldwide, and chances are you’ve experienced it at some point – remember that “stomach bug” that kept you close to the bathroom?
Bacterial Infections
The most common troublemakers include:
– E. coli (often from contaminated food)
– Salmonella (that undercooked chicken strikes again!)
– C. difficile (the notorious hospital-acquired infection)
– Campylobacter (frequently from raw poultry)
Typical symptoms include:
– Sudden onset diarrhea
– Stomach cramps
– Fever
– Nausea and vomiting
– Blood in stool (in severe cases)
Viral Infections
Think of viral colitis as the sneaky cousin of bacterial infections. Common culprits include:
– Norovirus (the cruise ship virus)
– Rotavirus (more common in children)
– Cytomegalovirus (particularly in immunocompromised individuals)
Parasitic Infections
These unwanted visitors typically cause:
– Prolonged diarrhea
– Abdominal pain
– Weight loss
– Fatigue
– Nutrient deficiencies
Travel Alert:
> Traveling to developing countries? Pack that hand sanitizer! About 40% of traveler’s diarrhea cases are actually a form of infectious colitis.
Chemical and Radiation-Induced Colitis: The Environmental Impact
Sometimes colitis isn’t caused by any living organism but rather by external factors that irritate or damage the colon. Think of it as your colon getting a sunburn from the inside – ouch!
Chemical Colitis
Common causes include:
– Harsh enemas or colon cleansing products
– Accidental ingestion of chemicals
– Exposure to certain cleaning products
– Some contrast materials used in medical imaging
Symptoms typically include:
– Immediate onset of pain
– Burning sensation
– Bloody diarrhea
– Mucus in stool
Radiation Colitis
This type occurs in some patients undergoing radiation therapy for:
– Prostate cancer
– Cervical cancer
– Other pelvic cancers
The effects can be:
– Acute (during treatment)
– Chronic (developing months or years later)
– Progressive if not properly managed
Diversion Colitis: The Lonely Colon Syndrome
Here’s something fascinating – when part of the colon is surgically bypassed (like with a temporary colostomy), the unused portion can become inflamed. It’s as if your colon gets lonely and upset when it’s not doing its job!
Key features:
– Occurs in surgically bypassed colon segments
– Develops within weeks to months after surgery
– Often improves when intestinal continuity is restored
– Can cause bleeding and mucus discharge
– May be asymptomatic in some cases
Allergic and Eosinophilic Colitis: When Your Immune System Overreacts
Sometimes your immune system can be a bit like an overprotective parent – reacting dramatically to things that shouldn’t really be a threat.
Allergic Colitis
Most common in infants:
– Often related to milk protein allergy
– Can be triggered by other food allergens
– Usually resolves with allergen elimination
– Causes bloody stools in otherwise healthy babies
– May require dietary changes in breastfeeding mothers
Eosinophilic Colitis
A rare but distinct condition:
– Characterized by high levels of eosinophils (white blood cells)
– Can affect any age group
– Often associated with other allergic conditions
– May require specialized treatment approaches
– Can be difficult to diagnose
Drug-Induced Colitis: When Medicine Has Side Effects
Sometimes the very medications meant to help us can cause problems of their own. Drug-induced colitis is like friendly fire in the battle for health.
Common culprits include:
– NSAIDs (like ibuprofen and aspirin)
– Antibiotics
– Some cancer medications
– Immune checkpoint inhibitors
– Birth control pills
Characteristics:
– Usually improves when medication is stopped
– Can mimic other forms of colitis
– May require medication changes
– Sometimes needs additional treatment
– Can be prevented with proper medication management
Medication Alert:
> Taking NSAIDs regularly? Talk to your doctor about protective strategies for your colon. Studies show that up to 70% of long-term NSAID users develop some degree of colitis.
Prevention and Management Tips
While not all forms of non-IBD colitis are preventable, you can reduce your risk:
1. Practice good food safety
2. Wash hands frequently
3. Be careful with medications
4. Stay hydrated
5. Follow radiation therapy protective protocols
6. Get immediate care for symptoms
Remember, most forms of non-IBD colitis are temporary and treatable. The key is getting proper medical attention and following through with recommended treatments. Unlike IBD-related colitis, many of these forms can be completely cured with appropriate intervention.
When to See a Doctor
> Don’t wait if you experience:
> – Severe abdominal pain
> – High fever
> – Significant bleeding
> – Signs of dehydration
> – Symptoms lasting more than a few days
You want us to discuss more on how to live well with Colitis as we did with living with IBS, follow for more!